By Georgia Barrington-Smith & Dr Rebecca Duncan
Medical radiation procedures, such as diagnostic imaging and radiation therapy, are critical in modern healthcare, providing life-saving detection and treatment tools for people suffering from diseases like cancer. Recent technological advancements have led to a new generation of radiotherapy treatments that promise to further enhance patient outcomes.
Developing radiotherapies
Unlike traditional radiation therapies that use large beams with broad target areas, microbeam radiation therapy (MRT) uses tiny, highly focused beams for more precise treatment. Unfortunately, traditional detection equipment cannot keep up with the steep dose changes and high intensities of MRT treatments; the small size and high intensity of the beams presents a considerable challenge in accurately measuring the amount of radiation being delivered to the patient. Therefore, there is a need to design a new generation of sensors with three key considerations:
- Ultra-fine spatial resolution (down to the micron level),
- The ability to mimic tissue behaviour in the human body to ensure accurate measurements across varying radiation energies, and
- A high tolerance to radiation, ensuring the device remains functional even under the intense radiation levels associated with MRT.
Additionally, with real-time monitoring now mandatory in many countries to detect, evaluate, and correct radiation dose deviations during treatment, the sensors must be adaptable to the patient’s shape and provide immediate feedback.
Jessie helps develop highly specialised sensors
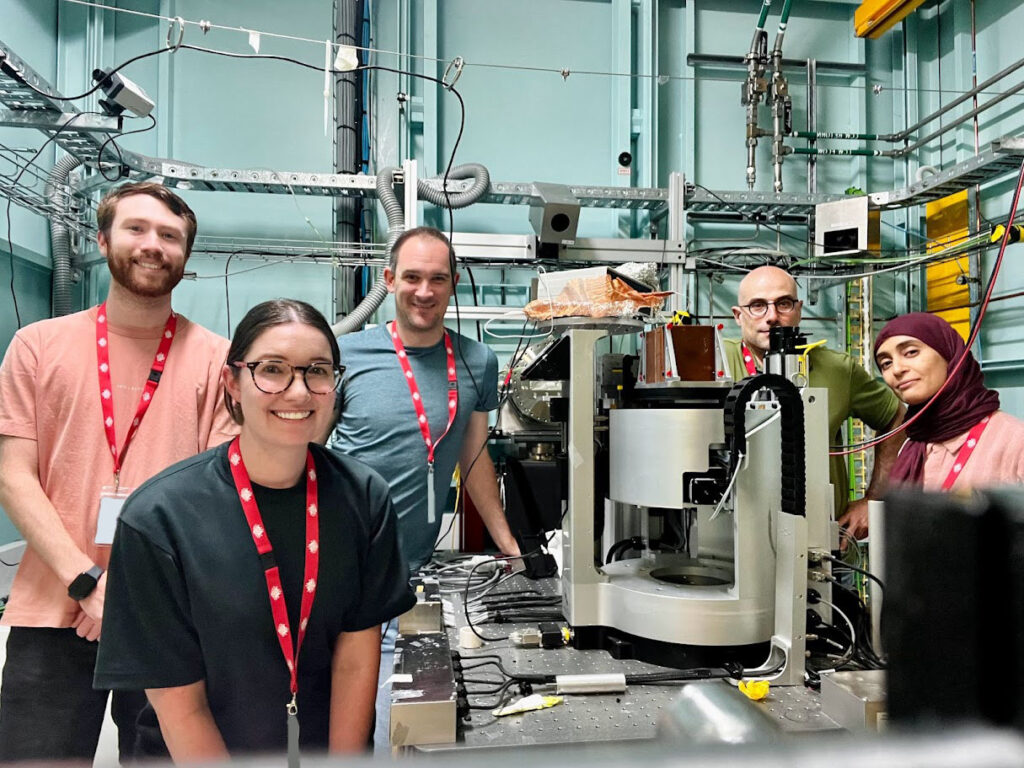
Consequently, Dr Jessie Posar, an AINSE ECRG recipient and 2022 AINSE Scholar Gold Medallist, along with her collaborators at ANSTO and the University of Wollongong, embarked on a research effort to develop wearable X-ray sensors that could monitor patients throughout their treatment to track radiation dosage.
The sensors were crafted from a carbon-based flexible material mounted on a specialised plastic film called Kapton, which was selected for its superior durability and flexibility compared to commercially-used polyethylene (PE). The sensor was designed with a very thin layer (260 nanometers thick, about 200 times thinner than a human hair) composed of two organic materials: P3HT (a polymer) and o-IDTBR (a special chemical compound). The sensor was connected to two types of metal contacts—Indium Tin Oxide (ITO) at the bottom and Aluminum at the top—to measure the X-ray signals.
To test the effectiveness of this new sensor, the team developed a custom-made system to read the sensor data in real time. The sensors’ response was then evaluated using the Imaging and Medical Beamline at ANSTO’s Australian Synchrotron, one of only two places in the world currently developing MRT technology.
Testing the feasibility of the X-ray sensor
Using multiple filters to adjust the energy of the X-ray beams to track the sensor’s responsiveness, the team discovered that when the sensor was mounted on Kapton film, it was sufficiently sensitive to accurately measure the required radiation doses with high spatial resolution. However, the team also detected that the Indium Tin Oxide layer was interacting with the incoming beam, which in turn negatively impacted the sensor’s performance.
Further testing revealed that using polyethylene instead of Kapton, caused the sensor to perform less efficiently because the current from the sensor flipped direction during testing, making it unreliable. They determined that the polyethylene caused a build-up of electrostatic charge at the interface between the polyethylene and the organic material, which interfered with the sensor’s performance. This problem was not present when Kapton film was used.
How robust is the sensor?
Next, the team tested how well the sensor could handle high levels of radiation. Overall, the sensor performed moderately well, showing a performance drop of approximately 35% when exposed to high doses. This is a significant improvement over previous radiation hardness studies on existing devices that showed performance decreases of 65%. This reinforced the new design as being more durable than pre-existing sensors.
Jessie’s research demonstrates the development of a new kind of sensor that could help make radiation treatments even more precise and safe. These sensors could improve future treatments for diseases like cancer by providing a means of monitoring the doses associated with new precise, high intensity therapies such as MRT, making the procedures safer and more effective.
AINSE are proud to spotlight Jessie Posar for her outstanding work!
To explore more incredible research by our AINSE scholars, visit ainse.edu.au/research-spotlight.
Don’t take your finger off the pulse as we bring you our next article in Medical March, showcasing the wonderful work of Samantha Alloo, who investigates the use of multimodal signals to uncover high-resolution details in clinical X-ray scans.
Stay up to date with AINSE by following us on all our social media platforms @ainse_ltd on Instagram, Facebook, Threads and LinkedIn.
